Patients with melanoma who have larger amounts of sentinel-node (SN) tumour burden and are negative on ultrasound (US)-guided fine-needle aspiration cytology (FNAC) can be spared an SN biopsy (SNB), but patients with peripheral perfusion and negative FNAC should proceed to undergo an SNB to detect microscopic occult disease, researchers stated at the 2015 Annual Meeting of the American Society of Clinical Oncology (ASCO). Patients who have completely negative US-FNAC might only require follow-up and no SN staging.
A retrospective study affirmed the wisdom of this step-wise approach, examining over 1,000 consecutive patients with stage I/II melanoma who underwent US-guided FNAC before sentinel-node biopsy (SNB) between 2001 and 2010.
In the case of positive FNAC and/or a case with clearly malignant ultrasound (balloon-shaped or loss of central echoes), patients have large amounts of sentinel-node burden, and poor survival is expected. These patients can be spared an SNB, according to lead investigator Alexander Christopher Jonathan Van Akkooi, MD, PhD, Netherlands Cancer Institute, Amsterdam, the Netherlands, and colleagues, whose poster was presented here on June 1.
US-FNAC has established value in the diagnostic work-up of breast and thyroid cancers. Its value in melanoma is less obvious, with poor sensitivities having being described; however, the introduction of the Berlin morphology criteria has boosted the sensitivity considerably, reaching 65% to 80% in some patients, and necessitates a revisit of its use in melanoma, noted Dr. Van Akkooi and colleagues.
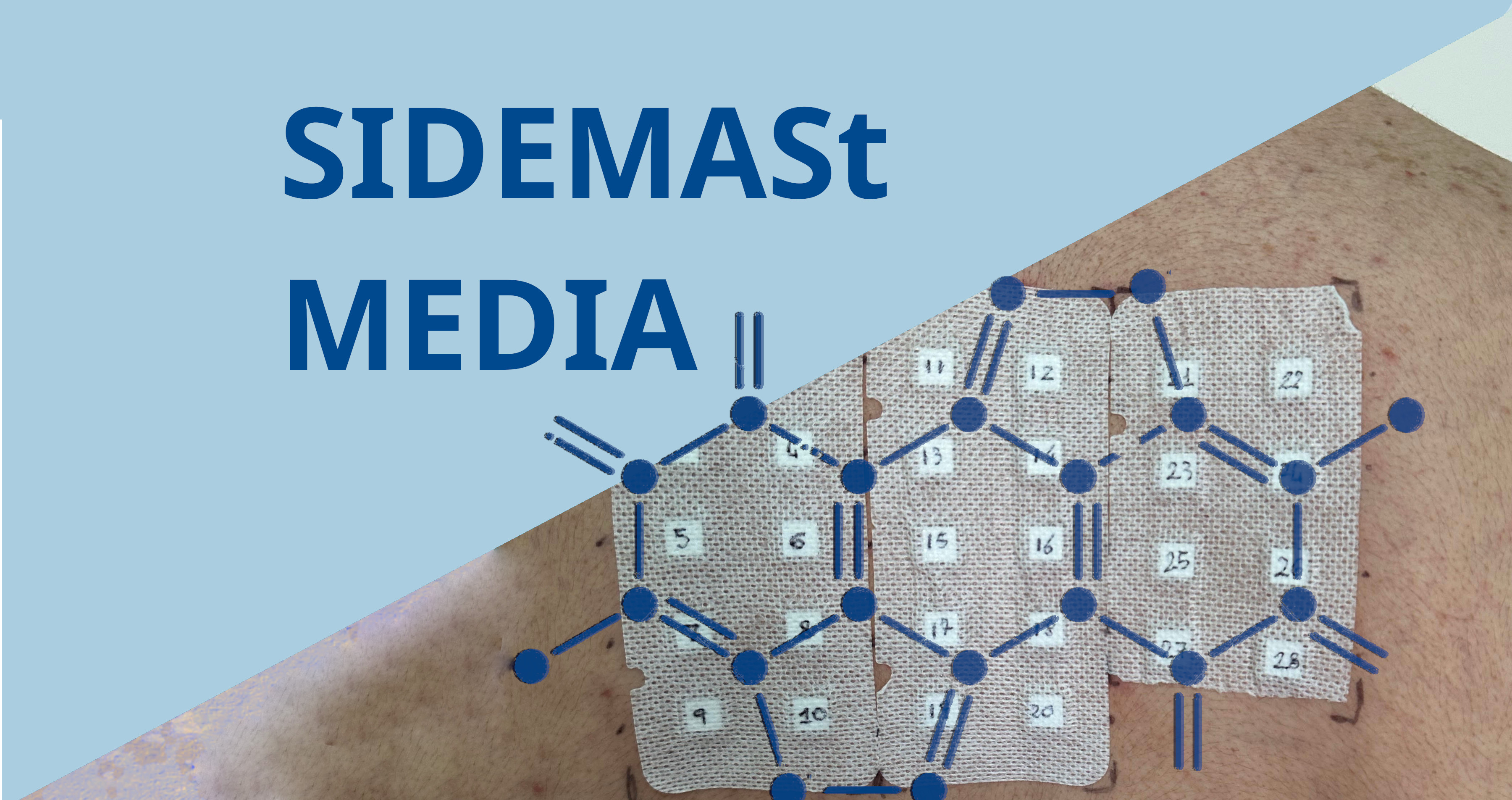
Their study involved patients with stage I/II consecutive melanoma in whom US-FNAC had been performed before SNB, with lymphoscintigraphy having been performed prior to the US-FNAC. FNAC was carried out if hallmarks of the Berlin criteria -- peripheral perfusion, loss of central echoes, and a balloon-shape -- were evident. The SN tumour burden was measured using the Rotterdam criteria. Positive FNAC results always prompted removal of SN or lymph node.
The mean/median follow-up was 69 months and 63 months, respectively (interquartile range: 42 to 98 months). The mean and median Breslow thickness were 2.58 mm and 1.57 mm, respectively. SN positivity rate was 21%. US-FNAC sensitivity was 71% for US and 51% for US-FNAC. US-FNAC sensitivity was maximal for T4 melanoma (76%) and ulcerated melanomas (63%). The sensitivity of peripheral perfusion, loss of central echoes, and a balloon shape were 69%, 24%, and 24%, respectively.
As the SN tumour burden increased, US-FNAC sensitivity increased. Peripheral perfusion was an early metastatic hallmark, being evident in 58% of small (< 0.1 mm) metastases. The threshold size of a metastasis for FNAC was 0.3 mm.
Compared with US-FNAC negative patients, patients with a positive FNAC result and/or presence of balloon shape or loss of central echo, poor survival was evident concerning melanoma-specific survival (hazard ratio [HR], 9.55; 95% confidence interval [CI], 6.66 to 13.59; P < .001), disease-free survival (HR, 9.12; 95% CI, 6.64 to 12.51; P < .001), and distant-metastasis-free survival (HR, 11.04; 95% CI, 7.77 to 15.69; P < .001).
Patients with peripheral perfusion and negative FNAC results had a slightly worse survival in terms of melanoma-specific survival (HR, 1.61; 95% CI, 1.06 to 2.44; P = .025), disease-free survival (HR, 1.45; 95% CI, 1.03 to 2.05; P = .034), and distant-metastasis-free survival (HR, 1.72; 95% CI, 1.16 to 2.55; P = .007) compared with completely negative patients, irrespective of the SN finding.
A positive US-FNAC result alone or along with the finding of balloon shape and/or loss of central echoes was associated with a significantly decreased melanoma-specific survival compared with patients who were US-FNAC-negative or those who displayed peripheral fusion but had not received FNAC (P < .001 and P = .025, respectively).
"In the case of peripheral perfusion and negative FNAC, patients should proceed to undergo a SNB to detect microscopic occult disease," the researchers concluded. "Completely US-FNAC-negative patients might only require follow-up and no SN staging."